Avoiding Adverse Drug Reactions: The Role of Pharmacogenomics
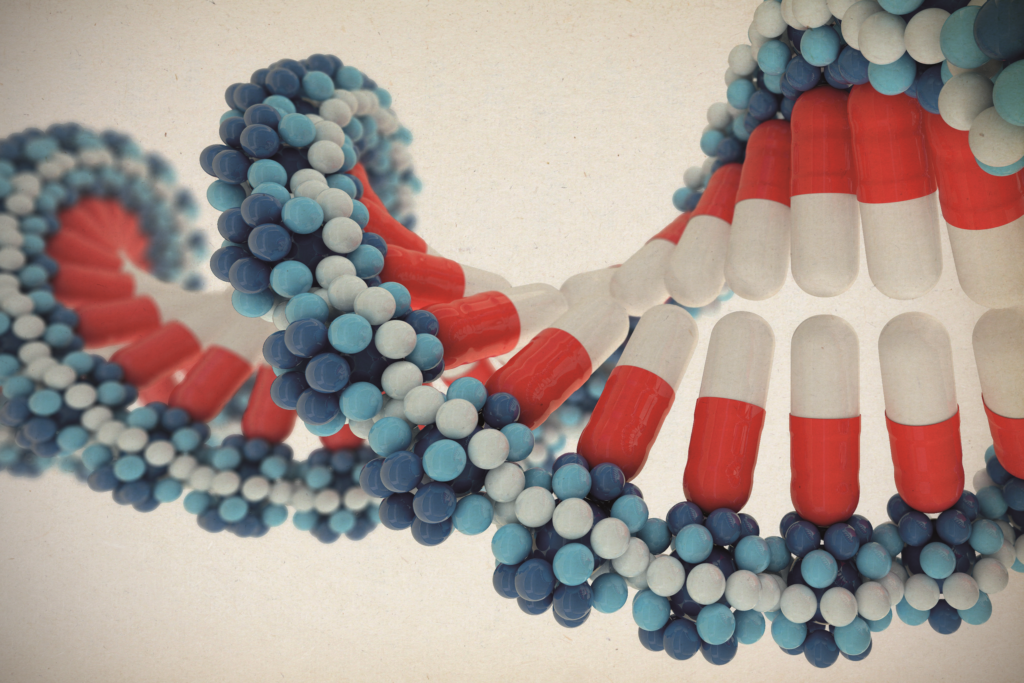
Every year, thousands of people suffer from adverse drug reactions—not because of the wrong diagnosis, but because the medication prescribed wasn’t right for their unique genetic makeup. Enter pharmacogenomics: a groundbreaking field that helps personalize drug therapy by considering how your genes affect your response to medications.
With advancements in precision medicine, healthcare is shifting away from one-size-fits-all treatments toward tailored solutions. The benefits of pharmacogenomics are becoming increasingly clear, especially when it comes to medication safety and efficacy.
What Is Pharmacogenomics?
Pharmacogenomics is the study of how genes influence an individual’s response to drugs. While some people may metabolize a medication quickly, others may process it too slowly, increasing the risk of side effects or reduced effectiveness.
By analyzing specific genetic variants, pharmacogenomic testing can help predict how your body will react to a particular drug—information that can guide doctors in prescribing the right drug for your genes.
Pharmacogenomics Benefits: Why It Matters
The benefits of pharmacogenomics are far-reaching and can significantly improve health outcomes. These include:
- ✅ Improved medication safety by reducing adverse drug reactions
- ✅ Faster recovery times through more effective prescriptions
- ✅ Fewer trial-and-error prescriptions, minimizing wasted time and resources
- ✅ Lower healthcare costs due to better-targeted treatment plans
- ✅ Enhanced patient trust and compliance with personalized care
One of the most impactful benefits is preventing dangerous side effects. For example, people with certain gene variants may experience life-threatening reactions to common drugs like codeine, warfarin, or antidepressants. Pharmacogenomic testing can identify these risks before the first dose is ever taken.
The FDA and Pharmacogenomics
The FDA recognizes the value of pharmacogenomics and has included pharmacogenetic information on the labels of over 250 drugs. This includes medications for cancer, heart disease, depression, and pain management. The FDA’s support underscores the growing importance of pharmacogenomic data in clinical decision-making.
Physicians can consult FDA guidelines to determine whether a pharmacogenomic test is recommended before prescribing a drug, ensuring treatments align with a patient’s genetic profile.
The Right Drug for Your Genes
Finding the right drug for your genes means choosing medications that work with your body—not against it. With a simple DNA test, healthcare providers can determine which drugs are likely to be effective or harmful based on your genetic makeup. This is especially valuable for patients who have experienced unusual side effects in the past or who are on multiple medications.
Pharmacogenomics is particularly useful in treating conditions like:
- Depression and anxiety (e.g., SSRIs, SNRIs)
- Cardiovascular diseases (e.g., beta blockers, statins)
- Pain management (e.g., opioids)
- Cancer therapies (e.g., chemotherapy agents)
Precision Medicine: The Future is Personal
Pharmacogenomics is a key pillar of precision medicine—a healthcare model that customizes treatment based on a person’s genetic, environmental, and lifestyle factors. This personalized approach not only improves patient care but also helps physicians avoid the risks of generic prescribing.
As more people undergo genetic testing, pharmacogenomics will play a greater role in everyday healthcare decisions, from routine prescriptions to complex treatment plans.
Conclusion
In a world where medication errors and adverse drug reactions are still all too common, pharmacogenomics offers a safer, smarter way forward. By using your genes to guide treatment, doctors can prescribe the right drug for your genes, reduce side effects, and enhance overall medication safety. Backed by FDA pharmacogenomics guidance and driven by the promise of precision medicine, this field is transforming how we treat and heal.
Whether you’re managing a chronic illness or just starting a new medication, consider asking your healthcare provider about pharmacogenomic testing. It could be the key to better health—with fewer risks.