Can Your DNA Influence Your Risk of Autoimmune Diseases?
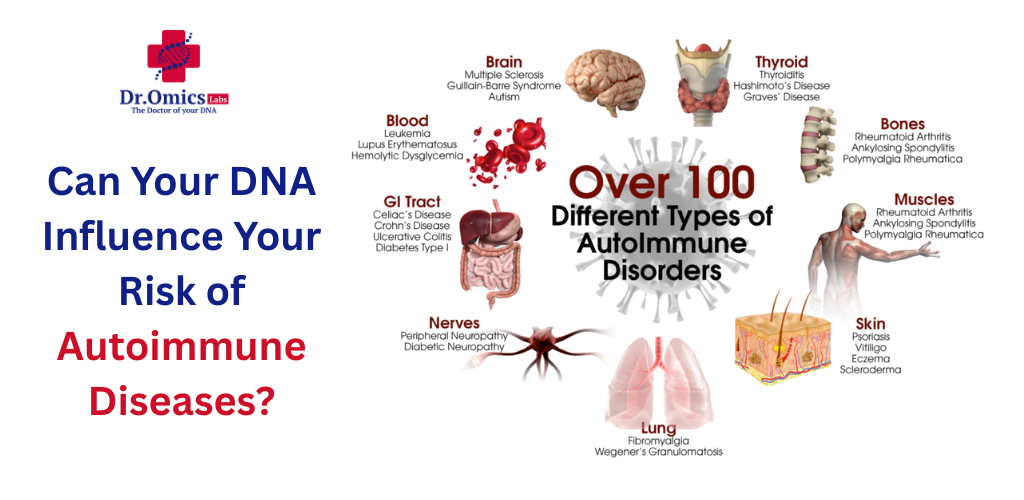
Autoimmune diseases have long puzzled researchers and patients alike. Why does the body suddenly start attacking its own tissues? And more importantly, could your DNA be the one pulling the strings behind the scenes? Thanks to breakthroughs in autoimmune disease genetics, we now know that your genetic code doesn’t just influence your eye color or height—it might also dictate how your immune system behaves, misbehaves, or breaks down entirely.
Genetics: The Unseen Puppeteer Behind Immune Disorders
Your DNA holds a deep archive of instructions, and some of those codes can set the stage for autoimmune conditions like lupus, rheumatoid arthritis, or multiple sclerosis. These aren’t random misfires of immunity—they’re increasingly being recognized as the result of genetic predisposition to lupus, faulty immune responses coded into our genomes, or inherited risks passed down over generations (2).
What’s even more fascinating—and alarming—is that rheumatoid arthritis DNA and multiple sclerosis genetics often show recurring patterns across families. Researchers have identified specific single nucleotide polymorphisms (SNPs) and mutations associated with these diseases. But here’s where it gets more interesting: the genes themselves are only part of the story.
Epigenetics: When Genes Don’t Change, But Behavior Does
It’s not just about which genes you inherit—it’s about how those genes behave. Through epigenetic modifications, such as DNA methylation, your body can silence or activate certain genes based on environmental exposures like toxins, infections, or even stress. These modifications don’t change the DNA sequence, but they can drastically alter immune function (1,4).
In diseases like systemic lupus erythematosus and rheumatoid arthritis, scientists have found that hypomethylated regions—sections of DNA stripped of chemical tags—can increase gene activity in T cells, potentially triggering an autoimmune attack (1). These findings bridge the gap between inherited risk and real-world triggers.
DNA: Friend or Intruder?
Ironically, your own DNA can sometimes act like an enemy. The immune system uses specialized pathways to detect foreign genetic material from viruses and bacteria. But in certain autoinflammatory diseases, this system mistakes your own DNA fragments—especially those leaked from damaged cells—as foreign invaders (2,3). That’s when the war begins.
This kind of mistaken identity can lead to constant immune activation, chronic inflammation, and irreversible tissue damage. In rare cases, mutations in DNA-sensing pathways can cause early-onset disorders like Aicardi-Goutières syndrome, offering critical insight into how personalized immune health must consider both genetic inheritance and regulatory mechanisms (2).
DNA Repair Gone Rogue
The body is equipped with complex DNA repair systems designed to fix genetic damage. But if mutations occur in genes responsible for DNA repair, it can result in unmanageable DNA fragments floating in the cytoplasm—yet another red flag for the immune system (3). These molecular “mistakes” may ignite or sustain autoimmune conditions, linking genetic damage directly to immune malfunction.
Researchers are now investigating whether interventions targeting the DNA damage response might one day curb or prevent disease onset. This is a new frontier in autoimmune disease genetics, where gene integrity and immune function are inseparably linked.
The Role of DNA Tests in Immune Health
So what does all this mean for you? With the rise of consumer genetics, it’s now possible to take a DNA test for immune health—a test that can reveal whether you carry certain risk alleles for common autoimmune diseases. For individuals with a family history of autoimmunity, this could provide early warning signs and allow for lifestyle changes or preventive care strategies tailored to your biology.
The future is clearly pointing toward personalized immune health, where diagnostics and treatments are based not just on symptoms but on your unique genomic fingerprint. It’s not science fiction. It’s happening right now.
The Genetic Bottom Line
Your immune system isn’t just a response system—it’s a complex symphony conducted by your DNA. Whether you’re carrying hidden mutations in rheumatoid arthritis DNA, differentially methylated genes linked to lupus, or subtle damage in DNA repair pathways, these invisible changes may be quietly altering your immune fate.
In short, your genetic predisposition to lupus, arthritis, or MS isn’t destiny—but it’s not a coincidence either. Understanding your genetic background could be the first and most powerful step toward preventing, managing, or even avoiding autoimmune diseases altogether.
References
- Funes, S. C., Fernández-Fierro, A., Rebolledo-Zelada, D., Mackern-Oberti, J. P., & Kalergis, A. M. (2021). Contribution of dysregulated DNA methylation to autoimmunity. International Journal of Molecular Sciences, 22(21), 11892. https://doi.org/10.3390/ijms222111892
- MacLauchlan, S., Fitzgerald, K. A., & Gravallese, E. M. (2022). Intracellular sensing of DNA in autoinflammation and autoimmunity. Arthritis & Rheumatology, 74(10), 1615–1624. https://doi.org/10.1002/art.42256
- Kivanc, D., & Dasdemir, S. (2021). The relationship between defects in DNA repair genes and autoinflammatory diseases. Rheumatology International, 42(1), 1–13. https://doi.org/10.1007/s00296-021-04906-3
- Fan, J. (2023). Investigation of DNA methylation in autoimmune diseases with genome-wide association analysis. ICMMGH 2023, 102. https://doi.org/10.1117/12.2692914