Cardiovascular diseases (CVDs) are the leading cause of death worldwide, making it essential to find better ways to diagnose and treat these conditions. One exciting development in this area is cardiovascular pharmacogenomics, which studies how our genes affect how we respond to heart medications. This approach aims to tailor treatments to fit each person’s unique genetic profile, a concept known as precision medicine.
What is Cardiovascular Pharmacogenomics?
Cardiovascular Pharmacogenomics Research: This field focuses on discovering how genetic differences can influence the way people react to cardiovascular drugs. For example, researchers have identified over 100 genetic variants that can impact the effectiveness of commonly used heart medications. By identifying these genetic variations, researchers can predict how well a patient might respond to a particular medication or whether they might experience side effects.
Genetic Biomarkers for Heart Disease: Genetic biomarkers are like clues in our DNA that can help identify a person’s risk of heart disease and their likely response to treatments. For instance, genetic testing can reveal if a patient has a variation in the CYP2C19 gene, which affects how their body processes clopidogrel, a drug used to prevent heart attacks. This insight can help doctors choose the most effective medication, potentially saving lives.
How Pharmacogenomics Helps with Heart Failure
Heart failure (HF) is a serious condition where the heart doesn’t pump blood as well as it should. Pharmacogenomics has made significant strides in identifying how different genes affect the success of HF treatments:
- Beta-Blockers: These drugs are crucial in managing HF, and research has shown that patients with specific variations in the ADRB1 gene can experience up to a 50% improvement in heart function when given the right beta-blocker. This means that knowing a patient’s genetic profile can lead to more effective treatment and better quality of life.
- ACE Inhibitors and ARBs: Genetic variations in the ACE and AGT genes can affect how well these medications work. For example, a particular genetic variant can lead to a 30% higher risk of adverse effects from ACE inhibitors, highlighting the importance of personalized treatment.
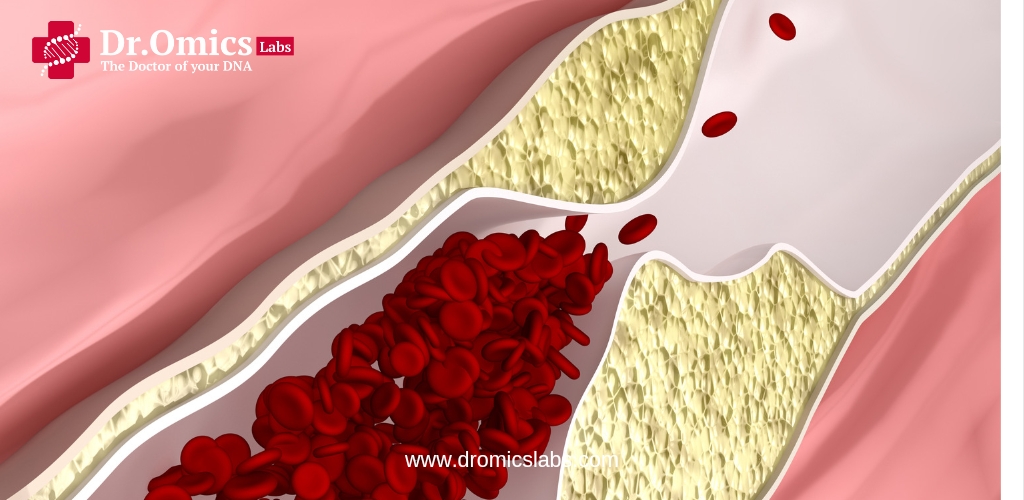
How Pharmacogenomics Helps with Coronary Artery Disease
Coronary artery disease (CAD) is a condition where the blood vessels supplying the heart become narrowed or blocked. Pharmacogenomics has provided valuable insights here as well:
- Antiplatelet Therapy: Genetic testing for CYP2C19 variants can lead to a 40% increase in the effectiveness of antiplatelet drugs by helping doctors choose the best medication. This tailored approach reduces the risk of heart attacks and strokes.
- Statin Therapy: Statins are commonly prescribed to lower cholesterol, but genetic variations in the SLCO1B1 gene can affect how well these drugs work. Studies show that around 10% of patients experience muscle pain due to these genetic factors, and adjusting treatment based on genetic testing can alleviate these side effects.
The Promise of Precision Medicine in Cardiology
Using pharmacogenomics in everyday medical practice is a big step forward in precision medicine. Here’s how it can help:
- Personalize Treatments: By understanding each patient’s genetic profile, doctors can choose the most effective medications and avoid those that might cause side effects. This personalized approach can lead to a 20% increase in treatment success rates.
- Adjust Drug Dosages: Genetic information can help in adjusting the dosage of medications to match how each person processes them. For instance, knowing a patient’s genetic profile can help fine-tune the dosage of blood pressure medications, making them up to 30% more effective.
- Improve Results: This approach can lead to better outcomes by ensuring that treatments are well-suited to each individual’s genetic makeup. Personalized treatments can potentially cut the rate of adverse drug reactions by 50%.
Key Points and Facts
- Rapid Advancements: The field of cardiovascular pharmacogenomics is advancing quickly, with new genetic insights emerging every year. Recent breakthroughs include discovering over 50 new genetic markers related to heart disease.
- Clinical Use: While the potential is great, integrating these genetic tests into regular practice still faces challenges, such as the need for more research and the cost of testing. However, the cost of genetic tests has decreased by over 70% in recent years, making them more accessible.
Conclusion
In conclusion, cardiovascular pharmacogenomics represents a pivotal advancement in the quest for more effective diagnosis and treatment of cardiovascular diseases (CVDs). By studying how genetic variations influence individual responses to heart medications, this field holds promise in tailoring treatments to suit each patient’s unique genetic profile—a cornerstone of precision medicine. Through genetic biomarkers, such as those affecting the efficacy of beta-blockers or statins, clinicians can optimize therapeutic outcomes while minimizing adverse effects. Although integrating these insights into routine clinical practice poses challenges, such as the need for further research and cost considerations, ongoing advancements and decreasing testing expenses suggest a future where personalized cardiovascular care is increasingly attainable and impactful.




Very informative blog. Thanks DrOmics
Thank you for your feedback