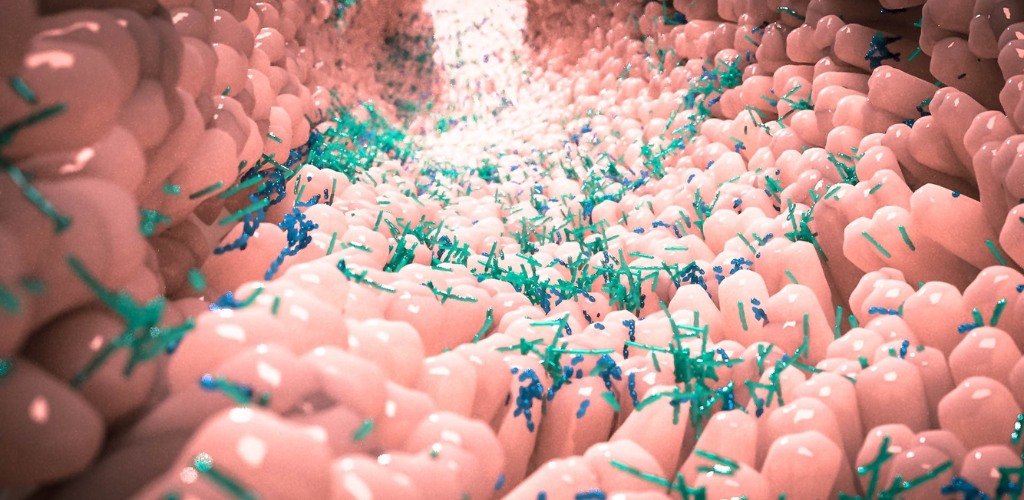
Human microbiome research focuses on understanding the diverse microbial communities that live in and on the human body, and their interactions with human hosts and their chemical environments. Key aspects of human microbiome research include:
- Sampling and analysis: Most microbiome analyses have focused on DNA or RNA sequencing, metabolomic analyses, or direct observation methods.
- Model organisms: Although no nonhuman model system can fully recapitulate all aspects of the human microbiome, each has distinctive strengths that can be leveraged to address specific scientific questions.
- Computational analyses: Computational analyses can complement any of the approaches discussed, such as epidemiology, animal, or in vitro studies.
- Human Microbiome Project (HMP): The Common Fund’s Human Microbiome Project (HMP) developed research resources to enable the study of microbial communities in the human body.
- NIH Human Microbiome Project: The NIH Human Microbiome Project focuses on characterising the microbiomes of healthy human subjects at five major body sites, using 16S and metagenomic shotgun sequencing.
- Human Microbiome Research Institute: The Human Microbiome Research Institute at Cedars-Sinai is a research and innovation hub for advancing discoveries in human microbiome science across clinical disciplines, with priority areas in cancer, early life, gastrointestinal diseases, metabolism, and autoimmunity.
- Microbiome-based research: The Human Microbiome Research Institute facilitates research across all clinical disciplines and specialties, with priority areas in cancer, early life, gastrointestinal diseases, metabolism, and autoimmunity.
Why is Human Microbiome is important to study ?
- Understanding human health: By understanding the microbial makeup of a healthy person, researchers can learn how microbes influence human health and disease.
- Developing new therapies: A more complete understanding of the diversity of microbes in the human microbiome could lead to new therapies, such as treating bacterial infections by growing more “good” bacteria.
- Preventing and treating diseases: Studying the human microbiome can help identify effective interventions with large reductions in the relative risk of atherosclerotic coronary heart disease (CHD).
- Creating supportive environments: Health policies that create conducive environments for making healthy choices affordable and accessible are essential for preventing and treating cardiovascular diseases
How does the human microbiome affect mental health ?
Research has shown that the human microbiome can have a significant impact on mental health. An imbalance of bacteria in the microbiome can have serious consequences when it comes to GI health and mental health. Studies have demonstrated differences between subjects with psychiatric disorders and healthy controls in the composition of their gut microbiome. Dysbiosis and inflammation of the gut have been linked to causing several mental illnesses including anxiety and depression. The gut-brain axis is a bidirectional communication network that links the enteric and central nervous systems, allowing the brain to influence intestinal activities, including activity of functional immune effector cells; and the gut to influence mood, cognition, and mental health. Probiotics have the ability to restore normal microbial balance, and therefore have a potential role in the treatment and prevention of anxiety and depression. In conclusion, the human microbiome can have a significant impact on mental health, and further research is needed to better understand the mechanisms underlying this relationship and to develop effective interventions.
What are some of the potential applications of microbiome-based Cure ?
- Establishing a healthy gut environment: Microbiome therapy aims to establish a native gut microbial environment for healthy gut functioning and preventing dysregulation1.
- Overcoming drawbacks of conventional therapies: Microbial therapy can overcome drawbacks of modern medicines, such as antibiotic resistance among pathogens, resistance to chemotherapy, drug non-responsiveness, and poor specificity1.
- Personalised and sustainable treatment: Microbiome-based therapeutics provide personalised, harmonised, reliable, and sustainable treatment, overcoming the limitations of conventional therapeutics1.
- Treatment of various diseases: Microbiome-based therapies have potential applications in the treatment of various diseases, including infection, inflammatory diseases, oncology, autoimmune conditions, and central nervous system conditions.
- Dietary interventions, probiotics, and prebiotics: Microbiome-based therapies include dietary interventions, probiotics, prebiotics, antibiotics, phage therapy, faecal microbiota transplantation (FMT), live biotherapeutics, and microbiome mimetics, each aiming to modify the microbiome to treat diseases.
- Immunological consequences: Microbiome-based therapies can have immunological consequences and are being developed to treat diseases such as cancer, diabetes, allergy, obesity, and infection.
Conclusion :
In conclusion, human microbiome research aims to understand the diverse microbial communities that live in and on the human body, their interactions with human hosts, and their impact on human health. This research has the potential to lead to new insights and interventions for various health conditions.
Citations:
[1] https://www.ncbi.nlm.nih.gov/books/NBK481559/
[2] https://commonfund.nih.gov/hmp
[4] https://www.cedars-sinai.edu/research/departments-institutes/human-microbiome-research.html
[5] https://www.nature.com/articles/s41467-020-18983-8